
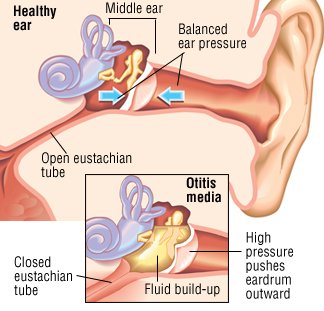
Ear infections most often develop after a viral respiratory tract infection, such as a cold or the flu. These infections can cause swelling of the mucous membranes of the nose and throat, and diminish normal host defenses such as clearance of bacteria from the nose, increasing the amount of bacteria in the nose. Viral respiratory tract infections also can impair Eustachian tube function. Normal Eustachian tube function is important for maintaining normal pressure in the ear. Impaired Eustachian tube function changes the pressure in the middle ear (like when you are flying in an airplane). Fluid (called an effusion) may form in the middle ear and bacteria and viruses follow, resulting in inflammation in the middle ear . The increased pressure causes the eardrum to bulge, leading to the typical symptoms of fever, pain, and fussiness in young children.
EAR INFECTION SYMPTOMS
Symptoms of an ear infection in adolescents and older children may include ear aching or pain and temporary hearing loss. These symptoms usually come on suddenly.
In infants and young children, symptoms of an ear infection can include:
Fever
Pulling on the ear
Fussiness or irritability
Decreased activity
Lack of appetite or difficulty eating
Vomiting or diarrhea
EAR INFECTION DIAGNOSIS
If you suspect that your child has an ear infection, call your doctor or nurse to see if and when the child should be examined.
Although the exam is not painful, most infants and children do not like having their ears examined. To make the process easier, hold your child in your lap and hug your child's arms and body while the doctor or nurse uses an instrument (otoscope) to look inside the child's ear. Often cerumen (ear wax) will need to be removed so your doctor or nurse can get a good view of the ear drum.
The doctor or nurse can tell if your child has an ear infection by looking at the ear drum (tympanic membrane) for the typical features of an ear infection.
EAR INFECTION TREATMENT
Treatment of an ear infection may include:
Antibiotics
Medicines to treat pain and fever
Observation
A combination of the above
The "best" treatment depends on the child's age, history of previous infections, degree of illness, and any underlying medical problems.
Antibiotics — Antibiotics are usually given to infants who are younger than 24 months or who have high fever or infection in both ears. Children who are older than 24 months and have mild symptoms may be treated with an antibiotic or observed to see if they improve without antibiotics.
Antibiotics can have side effects such as diarrhea and rash, and overusing antibiotics can lead to more difficult to treat (resistant) bacteria. Resistance means that a particular antibiotic no longer works or that higher doses are needed next time.
Observation — In some cases, your child's doctor or nurse will recommend that you watch your child at home before starting antibiotics; this is called observation. Observation can help to determine whether antibiotics are needed.
Observation may be recommended in these situations:
If the child is older than 24 months
If ear pain and fever are not severe
If the child is otherwise healthy
You can give pain-relieving medicines during observation to ease pain. (See 'Pain management' below.)
If your child is being observed rather than treated with antibiotics, you will need to call or go back to the doctor or nurse's office after 24 hours for follow-up. If your child's pain or fever continues or worsens, antibiotics are usually recommended; observation may continue if the child is improving.
Pain management — Pain-relieving medicines, including ibuprofen (sample brand name: Motrin), acetaminophen (sample brand name: Tylenol), or ear drops (sample brand name: Auralgan) that contain a numbing medicine, may be used to reduce discomfort.
Complementary and alternative medical treatments — There are a wide variety of complementary and alternative medical (CAM) treatments advertised to treat ear infections. These may include homeopathic, naturopathic, chiropractic, and acupuncture treatments.
There are few scientific studies of CAM treatments for ear infection, and even fewer studies that show CAM treatments to be effective. As a result, these treatments are not recommended for ear infections in children.
Decongestants and antihistamines — Cough and cold medicines (which usually include a decongestant or antihistamine) have not been proven to speed healing or reduce complications of ear infections in children. In addition, these treatments have side effects that can be dangerous. Neither decongestants nor antihistamines are recommended for children with ear infections.
Follow-up — Your child's symptoms should improve within 24 to 48 hours whether or not antibiotics were prescribed. If your child does not improve after 48 hours or gets worse, call your doctor or nurse for advice. Although fever and discomfort may continue even after starting antibiotics, the child should get a little better every day. If your child appears more ill than when seen by his or her health care provider, contact the provider as soon as possible.
Children who are younger than two years and those who have language or learning problems should have a follow-up ear exam two to three months after being treated for an ear infection. These children are at risk for delays in learning to speak. This follow-up helps to ensure that the fluid collection (which can affect hearing) has resolved. (See 'Ear infection complications' below.)
EAR INFECTION COMPLICATIONS
Tympanic membrane rupture — One of the common complications of an ear infection is rupture of the ear drum, also known as the tympanic membrane. The tympanic membrane can rupture when fluid presses on the membrane, reducing blood flow and causing the tissue to weaken. It does not hurt when the membrane ruptures, and many children actually feel better because pressure is released. Fortunately, the tympanic membrane usually heals quickly after rupturing, within hours to days. Rupture of the ear drum is an indication for antibiotic treatment of an ear infection.
Hearing loss — The fluid that collects behind the eardrum (called an effusion) can persist for weeks to months after the pain of an ear infection resolves. An effusion causes trouble hearing, which is usually temporary. If the fluid persists, however, it can interfere with the process of learning to speak.
Effusions usually resolve without any treatment. However, if the effusion persists for more than three months, the child may need treatment with a surgical procedure. The decision to treat is based upon how much the effusion affects the child's hearing and the child's risk of speech problems.
Children who are not treated for an effusion should be monitored over time. This includes an ear exam and hearing testing every three to six months until the effusion goes away.
EAR INFECTION PREVENTION
Some children develop ear infections frequently. Recurrent ear infections are defined as three or more infections in six months, or four or more infections within 12 months. In addition to receiving the pneumococcal and influenza vaccines, as recommended for all children, several interventions can help reduce the risk of recurrent infections. These include avoidance of tobacco smoke, breastfeeding, continuous low dose antibiotics, and/or surgical placement of tubes in the ears.
Preventive antibiotics — Children who have recurrent ear infections are sometimes treated with a preventive regimen of a daily antibiotic during the fall, winter, and early spring months. Although preventive antibiotics might help reduce the number of ear infections, it is still possible for the child to get an infection. There is also a risk that taking antibiotics for a long period of time can lead to bacteria that are resistant to standard antibiotics. Talk to your child's doctor or nurse about the potential benefits and risks of this approach.
Surgery — Some studies show that having surgery to place tympanostomy tubes in the ears helps to prevent recurrent ear infections. Other studies show no benefit of tympanostomy tubes for prevention of recurrences. Talk to your child's doctor about the risks and benefits of surgery.

No comments:
Post a Comment